If you are a preceptor or rotation coordinator who completes an In Training Assessment Report (ITAR) on One45’s WebEval system; thank you!! Your narrative comments are invaluable.
The Family Medicine In-Training Assessment Reports (ITARs) are critical for the program to be able to make decisions on progress and advancement. Ideally, the ITAR process consists of a brief face-to-face discussion with the resident near the start of the rotation to discuss learning goals, resident progress discussed at the middle of the rotation, and at the end of a rotation, followed by completion of the End of Rotation ITAR. We advise residents to prompt you to set up a time to meet in advance of the rotation. The ITAR is part of the resident’s permanent record in the program.
This web page will walk you through the process from start to finish
A short discussion with you at the start, to sketch out learning for the rotation is very appreciated by Residents.
We ask Residents to note their learning goals on the Goal Setting ITAR (or equivalent). These should be automatically sent to you by One45.
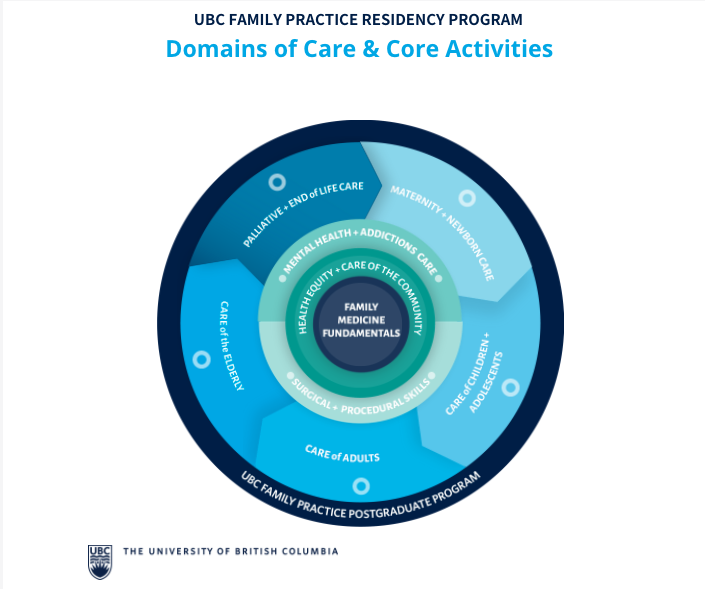
Resident goals are based on:
- the resident's unique needs,
- the relevant Core Learning Outcomes or site-specific objectives for the rotation,
What you add to the discussion are:
- Relevant learning goals based on what your rotation can likely offer.
- What do you and other preceptors note the resident needs as the rotation progresses.
Sketch out a plan for learning that is appropriate for the length of the rotation.
- For a 2 week rotation – consider 2-3 learning goals.
- For a 4 week rotation – consider 4-6 defined goals.
- You and the resident may adjust the goals as needed.
If all is going well, and the rotation is
- a block of 4 weeks or less, or
- less than 3 months if horizontal or longitudinal,
then having a discussion halfway through such that the resident is aware of their progress is important.
A written Mid-Point ITAR documenting the discussion between you and the resident must be used for these specific circumstances:
- every 3 months for horizontal rotations,
- if the block rotation is greater than 4 weeks, or
- regardless of length, if the resident is not progressing as expected.
All ITARs are informed by:
- Multiple observers via Field Notes, end of shift forms, and similar;
- In-person (direct) observation of resident performance;
- Discussion with colleagues, including allied health professionals;
- Review of cases, and;
- Review of progress notes and other clinical documentation.
The faculty responsible for the completion of the ITAR may ask the resident to forward Field Notes or End of Shift forms to use as an "aide mémoire" to inform the ITAR.
Objectives:
- give guidance as to what might be learned during a learning event.
- should be available at most sites for each rotation.
As the curriculum in residency is "what walks in the door" there is no guarantee that any resident may the opportunity to meet all objectives.
Your assessment of resident performance is what lets us know if a resident is competent in your rotation's context, not the completion of "all objectives".
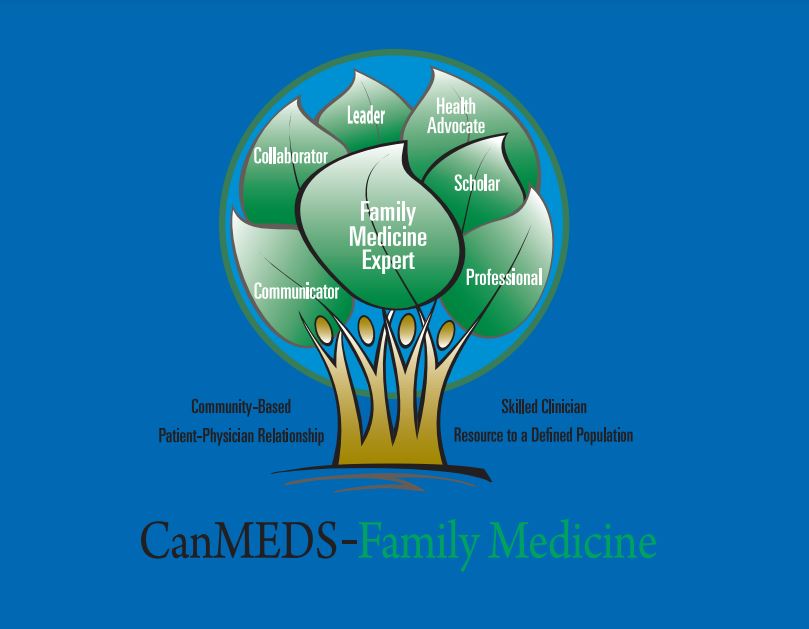
The UBC Family Medicine ITAR is currently based on the CanMEDS-FM roles.
What helps:
- Your sense of how a resident is doing overall in each role
- In the ITAR, click on the role to see a description.
- Your rich description of resident performance in these roles
- what are the strength of this resident
- What needs improvement, overall for this resident
To be more specific with your narrative on the ITAR, go to the section on "What are the Assessment Objectives and do they have a place on the ITAR?
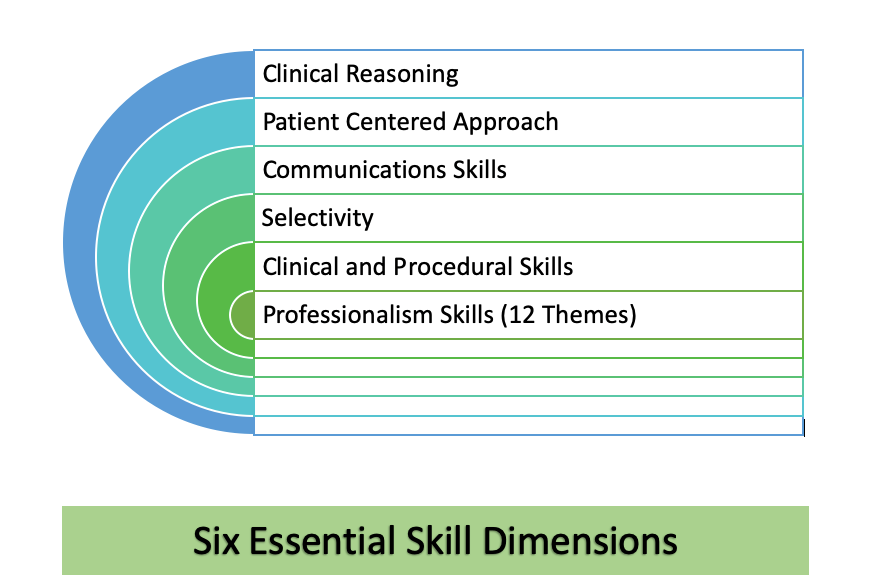
The Assessment Objectives consist of:
- 6 Essential Skill Dimensions
- Core Priority Topics (PT) and associated Key Features.
There are additional Priority Topics and Key Features for:
- Intrapartum and Newborn Care
- Rural and Remote Family Medicine
- Mental Health (in addition to those in the Core PT)
Priority Topics are common presentations that our graduates should be able to manage, and designed to give specific assessment points for these presentations.
The 6 Essential Skill Dimensions are skills used to manage and resolve clinical presentations that every resident needs to master and are assessable across:
- all clinical domains,
- academic and educational domains, (Professionalism Skills, Communications Skills).
The Key Features for each Priority Topic spell out specific points for assessment of competence. These are carefully chosen to address:
- what is difficult,
- what is critical to do, and
- where do physicians often make mistakes.
Mastery of Key Features gives reassurance of competence. It is unrealistic that Residents would encounter and be assessed on every Priority Topic, so we ask that they identify and target their gaps, and focus on these for assessment.
We know good residents do this spontaneously!
The CanMEDS-FM roles and the 6 Skill Dimensions do fit together. This mapping is an indication of how these frameworks integrate.
| CanMEDS-FM Role | 6 Skill Dimensions |
| Family Medicine Expert | Clinical Reasoning |
| Communicator | Communications Skills
Patient-Centered Approach Selectivity |
| Collaborator | Communications Skills (Effective Communication with Colleagues)
Professionalism (especially Theme 7) |
| Leader | Clinical Reasoning
Selectivity Communications Skills |
| Health Advocate | Communications Skills (especially Effective Communication with Patients) |
| Scholar | Professionalism Skills Theme 9 |
| Professional | Professionalism Skills – all Themes |
Please go ahead and flag a CanMEDS-FM Role (at least) if you are unsure, at all concerned, or think the resident really needs more time in a particular context.
It might feel difficult to "flag" an overall "does not demonstrate competence". Know that when you do this the first thing that happens is:
- The site get alerted to this need
- The resident gets support.
Next time you fill in the ITAR click on the links for more information.
The resident can appeal ITARs based on substantive issues of the process that affect the fairness of the assessment.
The most common reason for the appeal of an ITAR:
- not clearly hearing that you had concerns about their performance during the rotation.
- Significant delay in filling in an ITAR
This is why a written Midpoint ITAR is required if performance concerns are noted!
Residents need at least 25% of the time left in rotation to demonstrate they are working to resolve any performance concerns.
Should an appeal of an ITAR you completed be successful, your concerns as noted in the narrative, are not ignored. The responsible Competency Committee must still support the resident to mitigate your concerns.
UBC Family Practice Residency Program in Training Assessment Report (ITAR) Appeal Policy
- Appeal Process
1.1 The resident may appeal an ITAR when the reporting preceptor has stated that the resident does not meet expectations overall at the end of a rotation.
1.2 The resident must communicate an intention to appeal to the program director, or designate, in writing, within fourteen (14) calendar days of being notified by One45 (or equivalent) of an ITAR which states there was a failure to meet expectations overall in the rotation.
1.3 The program director or designate will review the appeal and will determine whether the request for appeal is based on one of the grounds of appeal set out in this policy. If the request for appeal is not based on a ground of appeal set out in this policy the program director or designate may dismiss the appeal without further review.
1.4 The program director or designate can grant the appeal if conditions for appeal are
clearly met.
1.5 If the program director or designate is unable to determine whether conditions for
appeal have been met, they will forward the appeal to the Program Competency
Committee for review and decision.
1.6 If the original ITAR decision is reversed, either by the program director or designate, or the Program Competency Committee, the program director designate will amend the ITAR on one45 (or equivalent platform) in order to show the successful result of the appeal, with an explanation of why the appeal was successful. The original narrative of the ITAR as originally provided by the preceptor will remain unaltered.
1.7. If the appeal is denied, and the original ITAR decision is upheld, either by the program director or designate or Program Competency Committee, the resident will be informed in writing of this decision by the program director or designate.
- Grounds for Appeal
2.1. The reasons for failing to meet expectations are not pertinent to performance of the resident within the time frame of the actual clinical rotation.
2.2. The assessment information used to inform the ITAR was not from the preceptors or Allied Health Professional associated with the rotation.
2.3. The resident was not made aware of the performance concerns prior to the end of the rotation. This would include direct communication either in-person or virtually followed by some sort of written confirmation (email, midterm ITAR, or equivalent, or competency committee minutes).
2.4. For ITARs related to clinical experiences, the resident was not provided adequate time to address the performance issues. Adequate time is a minimum of 25% remaining in the clinical experience. If the program director or designate is unable to determine whether there was adequacy of time provided the decision will lie with the Program Competency Committee (see item 1.5)
2.5 The End Rotation ITAR documenting “Resident Not Meeting Expectations” was submitted greater than fourteen (14) calendar days from completion of the rotation in question
The items 2.1, 2.2, 2.3 2.4 and 2.5 are grounds for appeal and the presence of these do not guarantee success of the appeal.
- Consequences of Appeal
3.1. If an appeal is successful, the evaluative comments on the ITAR remain and an addendum is attached explaining the reasons for the successful appeal and reversal of the “not meeting expectations” decision.
3.2. If an appeal is successful or unsuccessful, further steps may be directed by the site-level competency committee (SLCC) and/or program competency committee (PCC).
*Reviewed and approved and by the PGEC on May 12, 2023*
Please inform your Site's program office promptly, and the ITAR will be re-directed.
Overall, use the CanMEDS-FM roles to tell us that a problem exists by flagging a role. Your narrative descriptions are very helpful. The ITAR has links to descriptions for each role. Describing specifically what you observed that concerned you is all that is needed.
The 6 Essential Skill Dimensions are useful for describing specific issues that you may observe.
Please also see the section on "What are the Assessment Objectives and do they have a place on the ITAR", for links to more detailed information, particularly on Professionalism Skills.