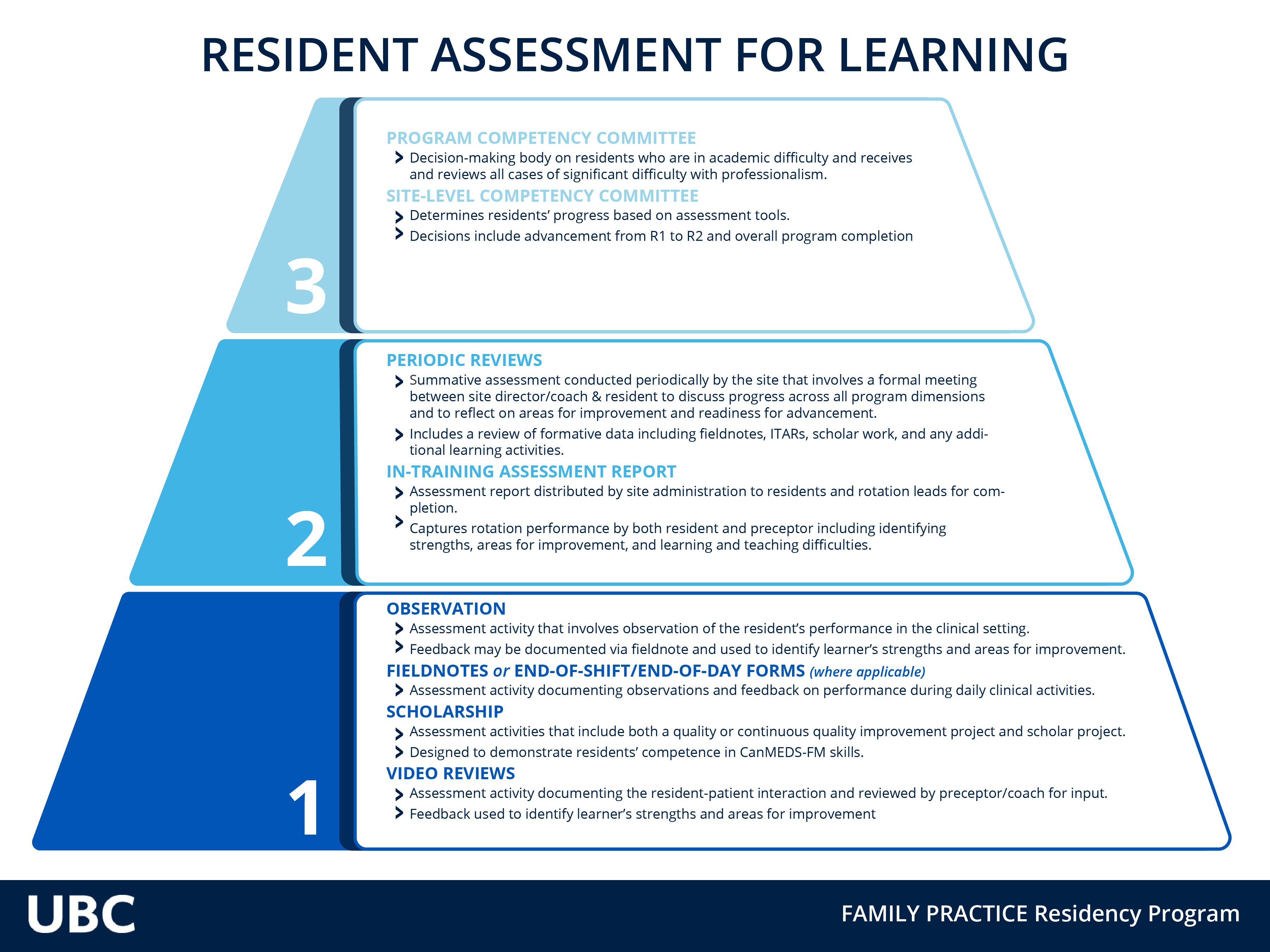
Resident Assessment for Learning
This graphic illustrates our tools, committees, and process that support our assessment for learning.
UBC Family Medicine Postgraduate Program Resident Assessment system is based on principles and practices of:
- Fairness,
- Transparency
- Being humanistic, and
- Evidence-informed
The Resident Assessment System embraces structure and processes that:
- Respects that each Resident comes with individual strengths and gaps
- Addresses the short length of training with an assessment strategy that both meets program expectations and is bespoke to the individual,
- Has a focus on metacognitive skills (e.g. self-awareness, self-regulation, guided self-reflection) as part of professional development.
- Is founded on the principles of programmatic assessment such that we look at the whole picture across the resident's training, using multiple low-stakes collaborative assessment points to inform decisions on progress and advancement.
- Prioritizes transparency and collaboration in both gathering of assessment information and in making decisions on progress.
We believe that this way of assessing performance best serves the developing professional family physician through deliberate practice, during residency, of skills that remain useful for life-long learning.
The programmatic assessment model for Family Medicine Programs across Canada is more fully explained in this document.
More Information for Preceptors
Stepping into the role of Preceptor, Coach, Assessor, and Supervisor is, like many new roles, full of jargon and concepts that may at first be unfamiliar, and are rapidly accrued. This short page offers a glossary of terms and brief explanations of the concepts that inform Assessment of Residents, to help speed that process for you.
First, know how much we (the program faculty, residents, and administrators) appreciate what you do every day as a preceptor, coach, and assessor. Thank you.
These roles are sometimes conflicting and challenging to manage, and an immensely valuable contribution to the training of family physicians in BC.
If you are new to these roles or are wishing to put some polish on your skills, this Faculty Development page may be helpful. Speak to your Site's Faculty Development person to discuss additional options.
As a preceptor, it is handy to know this background information as the robustness and trustworthiness of the decision on progress and advancement very much depends on your good quality assessment.
Jargon is both useful and sometimes frustrating and mysterious! Here is a glossary of terms you may find helpful.
The UBC Family Medicine Residency relies on a programmatic assessment model called Continuous Reflective Assessment For Training (CRAFT) to inform how assessment is done in our program.
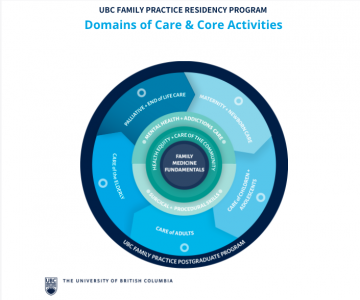
Competency-based programs need to be defined as Core Learning Outcomes. Our program has these described as 42 activities over 9 domains of care. These are activities that our graduates should be able to do. It is the scope of the work of a family physician at the point of embarking on independent practice.
Ensuring competence in a postgraduate program relies on:
- Direct observation,
- Multiple observers,
- Multiple observations
- Many different contexts.
- Coaching and documentation:
- residents and preceptors both contribute to Field Notes. (See Field Note Page)
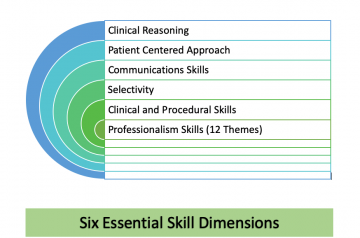
- Assessment of competence is primarily benchmarked against the College of Family Physicians of Canada's Assessment Objectives. The Assessment Objectives consist of:
- the Six Essential Skill Dimensions Preceptors use these skills every day and were the original source for the development of the 6 SD in Canada.
- Priority Topics with Key Features. Here is access to all the Priority Topics in individual pdf format. These are directly from the CFPC Assessment Objectives
- We also ask you to assess residents in the CanMEDS-FM roles. These broader roles are societal expectations of all Physicians, in this case, adapted for Family Medicine in Canada.
Linking the Core Learning Outcomes to Assessment Objectives:
Linking of CanMEDS-FM roles and Skill Dimensions to each of the Core Learning Outcomes is underway. This, along with comprehensive curriculum mapping will help to more concretely guide assessment for each learning opportunity.
In the interim, workplace-based assessment by skilled and competent observers, along with gap identification by residents, and coaching by a competency coach, already appropriately guides much of the assessment of residents and informs decisions on progress and advancement.
Direct Observation is defined here as a preceptor observing a resident in action. Often this is a resident interviewing a patient, but may also be observing a resident meeting with a family, or interacting with different members of the health care team. This differs from the case presentation where the resident is summarizing the clinical case and you are assessing the clinical content. You can and should directly observe the skill of giving a case presentation as this is an important communication skill.